Diet Quality Is Built Through Inclusion, Not Exclusion
Modern nutrition culture has slowly drifted towards restriction as the default. Foods are removed first, often before there is any clear plan for what replaces them. Dairy is excluded because it is labelled inflammatory. Gluten is avoided despite no diagnosed coeliac disease. Fruit is cut back in the name of blood sugar control. Entire food groups are sidelined in pursuit of simplicity, control, or perceived health optimisation.
The problem is that human physiology does not care about food rules. It cares about whether nutrient requirements are met, consistently and over time.
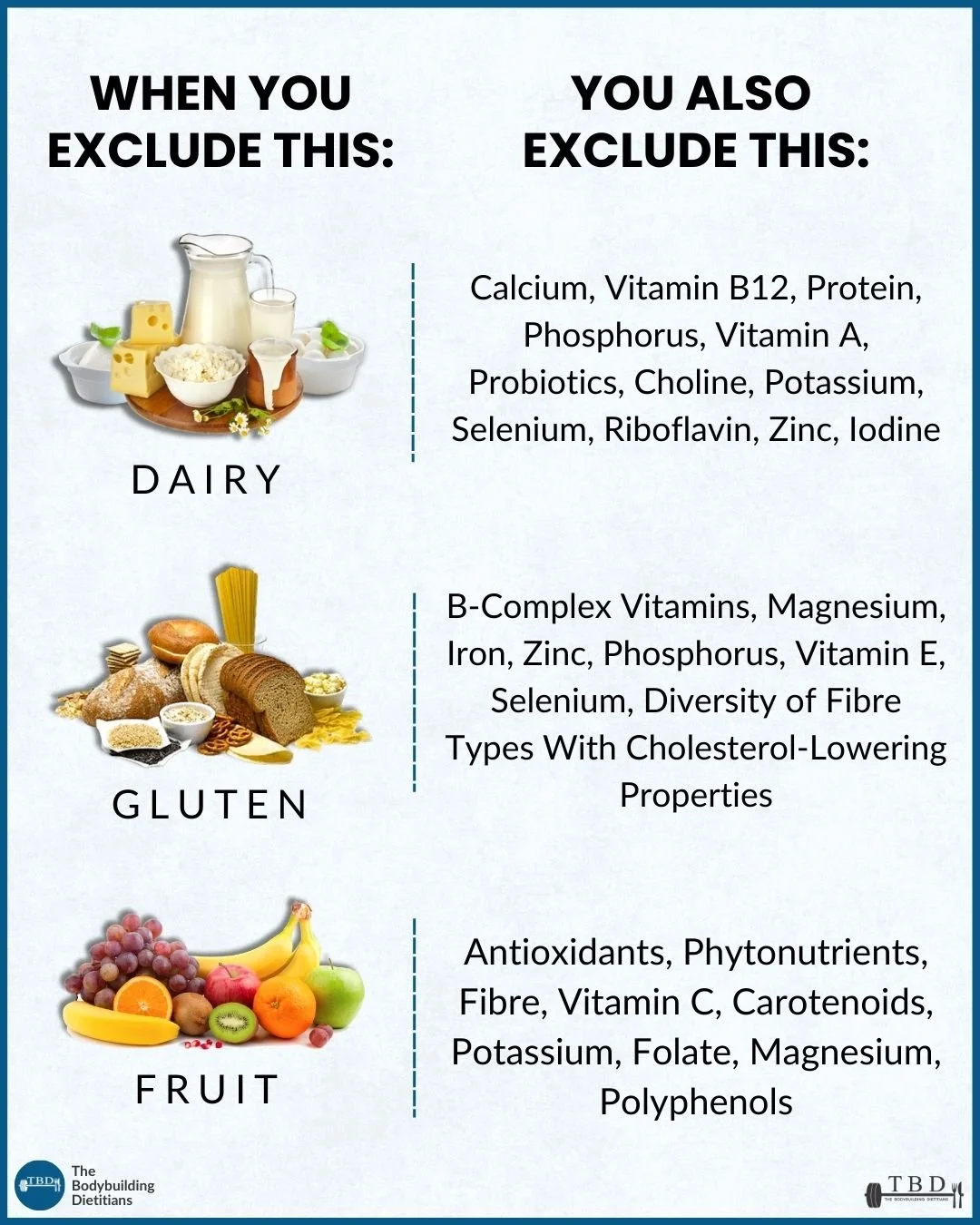
When foods are excluded from the diet, the consequence is not simply the absence of those foods themselves. What is also removed is the package of nutrients, bioactive compounds, and functional roles that those foods reliably provide. The more exclusions that accumulate, the narrower the nutrient pool becomes, and the greater the reliance on perfect planning, supplementation, or long-term dietary compliance to avoid gaps emerging.
Those gaps rarely show up immediately. Nutrient deficiencies are often slow, subtle, and cumulative. They tend to surface months or years later as reduced performance, compromised recovery, persistent fatigue, digestive issues, changes in bone health, or cardiometabolic markers that drift in the wrong direction. By the time they become obvious, the original dietary exclusions that contributed to them are often forgotten.
This is where the concept of inclusion becomes critical.
High diet quality is not built by obsessively removing foods. It is built by regularly including a wide range of nutrient-dense foods that naturally cover micronutrient needs without requiring constant tracking or supplementation. Diets that consistently include vegetables, fruits, wholegrains, legumes, lean proteins, dairy or fortified alternatives, nuts, and seeds tend to perform better across almost every long-term health outcome measured in population research.
Take dairy as an example. When dairy is removed without a clear replacement strategy, calcium intake often drops below recommended levels, alongside iodine, vitamin B12, riboflavin, potassium, phosphorus, and high-quality protein. In isolation, none of these changes may feel dramatic. Over time, however, they can meaningfully affect bone health, thyroid function, neuromuscular performance, and recovery.
Similarly, excluding gluten-containing grains frequently reduces intake of B-complex vitamins, magnesium, iron, zinc, selenium, and specific types of fermentable fibre that support gut health and cholesterol regulation. Many gluten-free alternatives are also lower in fibre and higher in refined starches, which can further shift dietary quality in unintended directions.
Fruit avoidance is another common example. While fruit is sometimes framed as optional or even problematic due to sugar content, its removal often reduces intake of vitamin C, folate, potassium, carotenoids, polyphenols, and diverse fibre types that play an important role in gut health, cardiometabolic risk reduction, and long-term disease prevention.
None of this is to suggest that food exclusion is inherently wrong. There are many valid reasons to remove certain foods, including allergies, intolerances, coeliac disease, inflammatory bowel conditions, ethical or religious beliefs, access limitations, or personal preference. Context always matters. The issue arises when exclusion is driven by fear, trends, or oversimplified nutrition narratives, without an understanding of what those foods contribute or how their role will be replaced.
A more resilient dietary approach starts with inclusion as the foundation. From there, exclusions can be layered in thoughtfully, with intentional substitutions that preserve nutrient adequacy. If dairy is removed, calcium-rich fortified alternatives, seafood, or specific plant sources need to step in. If gluten is excluded, attention must shift towards fibre-dense wholefoods and fortified grains that maintain micronutrient intake. If fruit intake is reduced, vegetables alone rarely fill the same nutritional role without very large volumes.
From a long-term perspective, the risk of developing a nutrient deficiency is far more consequential than consuming a food that has been unnecessarily framed as “bad.” The body is remarkably tolerant of individual foods eaten in moderation. It is far less tolerant of chronic insufficiency.
Good nutrition is rarely about perfection. It is about building a diet that is robust, flexible, and capable of meeting physiological needs across years, not weeks. Inclusion makes that process easier, more sustainable, and far less fragile.
If you want help building a diet that meets your nutritional needs without unnecessary restriction, our team works with individuals to create flexible, evidence-based nutrition plans that support performance, health, and long-term sustainability. You can learn more about our coaching and consultation options via the link below.